Heel pain can be caused by a variety of illnesses, such as plantar fasciitis and Achilles tendinitis. One typical symptom affecting the foot and ankle is a sore heel. Over time, pain can be reduced with the use of orthotics, rest, and stretching. Heel discomfort that is ignored or treated poorly may lead to chronic issues that require longer to repair. Seldom is surgery required to treat heel pain.
Overview
What is heel pain?
One typical issue with the feet and ankles is heel pain. Either behind or beneath the heel may pain. Heel discomfort can result from a variety of conditions, including:
- Plantar fasciitis.
- Bone spurs.
- Tendonosis or Achilles or flexor tendonitis.
- Bursitis.
- Inflamed tendons.
- Stress fractures.
- Sever’s disease.
In order to start the right treatment plan and identify the precise reason for your heel pain, it’s critical that you get a medical evaluation.
When you experience heel discomfort, it could be challenging to walk and go about your everyday business. Most painful heel problems can be resolved without surgery, but healing takes time.
How common is heel pain?
Every year, more than 2 million Americans deal with heel pain. The issue impacts individuals of all ages and genders.
Where does heel pain develop?
Anywhere in the heel, you could feel discomfort, soreness, or tenderness. Usually, you get heel pain:
1. Behind the heel.
2. Beneath the heel.
3. Within the heel bone itself.
What causes pain behind the heel?
The following issues can result in heel discomfort in the back of the heel:
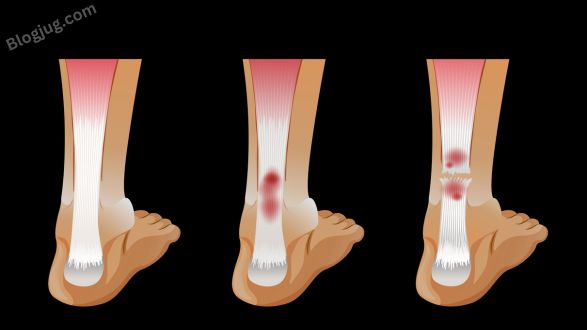
1. Achilles tendinitis: A fibrous band that joins the calf muscle to the heel bone is called the Achilles tendon. It is the strongest and longest tendon in the body. Basketball players and runners are more likely to get Achilles tendonitis. This overuse injury causes tendon inflammation. The back of the heel hurts, swells, and becomes stiff from tendinitis.
2. Bursitis: Bursa, are fluid-filled sacs that enlarge to cause bursitis. These sacs provide smooth movement by cushioning joints. The back of your heel may feel bruise-like and sensitive. Bursitis usually develops after extended periods of standing.
3. Haglund’s deformity: The formation of an enlarged bony bump at the back of the heel, known as a pump bump, can be brought on by persistent inflammation and irritation. Pumps and other shoes with higher heels might exacerbate the pain and bump.
4. Sever’s disease: Heel pain in active youngsters aged 8 to 14 is often caused by Sever’s disease. Kids who play sports that require a lot of running and jumping are more prone to this problem. The growth plate at the rear of the heel becomes irritated by the increasing physical activity.
What causes pain beneath the heel?
The following issues can result in pain beneath the heel:
1. Bone bruise: The fat that cushions the heel may get bruised if you step on something hard or sharp. Even though there might not be any discoloration, walking will cause your heel to feel uncomfortable. Both Sever’s disease and a stress fracture can hurt the heel all the way around, on the side, back, and bottom.
2. Plantar fasciitis: Heel discomfort is most commonly caused by plantar fasciitis. It happens when the fascia, or connective tissue, stretches or tears along the plantar area of the foot. This excruciating ailment is a more painful condition who run and jump a lot. Common sources of irritation include treadmills and hard surfaces (like concrete) used for work or exercise.
3. Heel spurs: A bony protrusion on the heel bone may develop as a result of persistent plantar fasciitis. Heel spurs are usually not painful, though some people report discomfort.
What are the risk factors for heel pain?
Heel pain can result from anything that places a lot of pressure and strain on the foot. Additional aspects include your foot’s shape (foot structure) and the way you walk (foot mechanics).
Heel discomfort may be more likely to occur if you:
1. Are overweight.
2. Possess high arches in their feet, flat feet, or arthritis in their ankles.
3. For fitness or in sports, run or jump a lot.
4. Stand for extended periods, especially on concrete floors.
5. Put on ill-fitting shoes that lack a cushion or arch support.
What are the symptoms of heel pain?
The causes and symptoms of heel pain can differ. Apart from discomfort, you could also feel:
1. Bony growth on the heel.
2. Discoloration.
3. Swelling.
4. Tenderness.
5. Stiffness.
6. Pain after rising from a seated or resting posture.
How is heel pain diagnosed?
In addition to evaluating your symptoms, your doctor will do a physical examination. X-rays can also be performed to look for joint deterioration, arthritis, bone fractures, and alignment issues in the bones.
You could infrequently require an ultrasound or MRI. These may disclose soft tissue issues that an X-ray is unable to pick up on.
What side effects might heel pain cause?
Your ability to move around, work, exercise, and perform daily duties may be hampered by heel pain. You may start to become sedentary when moving causes pain. Gaining weight can be a result of an inactive lifestyle. Being unable to do the things you enjoy doing could also make you feel down.
Achilles tendinitis can lead to tendon breakdown if left untreated. The Achilles tendon is prone to tearing or rupture over time. Surgery might be necessary to solve this issue.
How is heel pain managed or treated?
The majority of heel pain issues resolve on their own with nonsurgical therapies over time. Treatments aim to reduce stress and pressure on the heel, improve foot flexibility, and reduce discomfort and inflammation. Among these therapies are:
1. Injections: Injections of steroids can reduce inflammation and pain. Injections of steroids may be beneficial for plantar fasciitis and bursitis, but they should be used sparingly, if at all, for tendon problems.
2. Orthotic devices: Orthotics, which are custom-made or available over-the-counter, can relieve pressure on the heel. Wearing a splint at night can help some people, especially if they experience pain in the morning. For more severe symptoms, a walking boot could be required. For daily wear and exercise, you might also need to switch to more supportive footwear.
3. Pain relievers: Ice packs and nonsteroidal anti-inflammatory medication (NSAID) therapy reduce pain and swelling.
4. Physical therapy: Soft tissue adhesions can be broken up by ultrasound therapy, physical therapy, and massage. Pain and inflammation may be decreased by these treatments.
5. Stretching exercises: For stiff tendons and muscles, your healthcare provider can demonstrate heel stretching exercises.
6. Taping: Athletic or medical tape can be used to support the heel or arch of the foot.
Most heel pain causes can be treated without surgery very seldom.
How can I prevent heel pain?
It’s critical to maintain the flexibility of your foot and heel tendons to avoid heel discomfort or prevent it from returning. Stretching daily and wearing supportive, well-fitting shoes are recommended. Heel discomfort is particularly common among runners. Running on softer terrain and logging fewer miles will help you avoid running injuries.
What is the prognosis, for those experiencing heel pain?
Nonsurgical treatments usually relieve heel pain, but healing takes time. You must exercise patience and allow your body to heal. Resuming your regular activities too soon may hinder your recuperation. Rarely, you might require surgery.
When should I call the doctor?
You ought to contact your physician if you encounter:
1. Pain that doesn’t go away after taking medication or relaxing for a few weeks.
2. Pain that makes it hard to move or walk.
3. Severe stiffness, edema, or inflammation in the feet or stiffness.
What questions should I ask my doctor?
You should ask your medical professional:
1. What is causing my heel pain?
2. What is the best treatment for me?
3. How can I reduce my chance of experiencing heel discomfort in the future?
4. Which symptoms require a more immediate assessment?
A note from Blogjug
Nonsurgical therapies for heel pain frequently result in gradual improvement. Your medical professional can identify the source of your pain. In addition, your healthcare practitioner can demonstrate stretches for you and, if necessary, suggest orthotics and other treatments. Many attempt to ignore heel pain and carry on with activities that exacerbate the condition. However, you must allow your body enough time to heal. If not, you can experience persistent heel pain that keeps you from moving around for a long period. It’s critical to get checked since the harder it is to manage heel pain successfully the longer it persists.